Credentialing Services
Pro1RCM Provides Professional Medical Provider & Group Credentialing Services.
Pro1RCM Professional Credentialing Services
Credentialing is a critically important process for clinical providers and healthcare institutions. It is the process of reviewing and verifying the requisite academic qualifications and clinical practice history of a healthcare provider required by providing insurance companies prior to being eligible to receive reimbursement for medical Services provided to patients.
The Pro1RCM Credentialing Specialists are certified and highly-experienced professionals that can expertly and very efficiently navigate your Clinical Providers as well as your Practice (“Group”) through the rigorous steps, information gathering, and credentialing application process with each of the payer groups that your practice is contracted or looking to be contracted with.
The Pro1RCM Professional Credentialing Processes
Pro1RCM Credentialing Specialists serve as expert extensions of your practice, managing the entire primary source verification and enrollment processes, and expedites the completion of the credentialing process by allocating the necessary resources and continuously following on every step of the process.
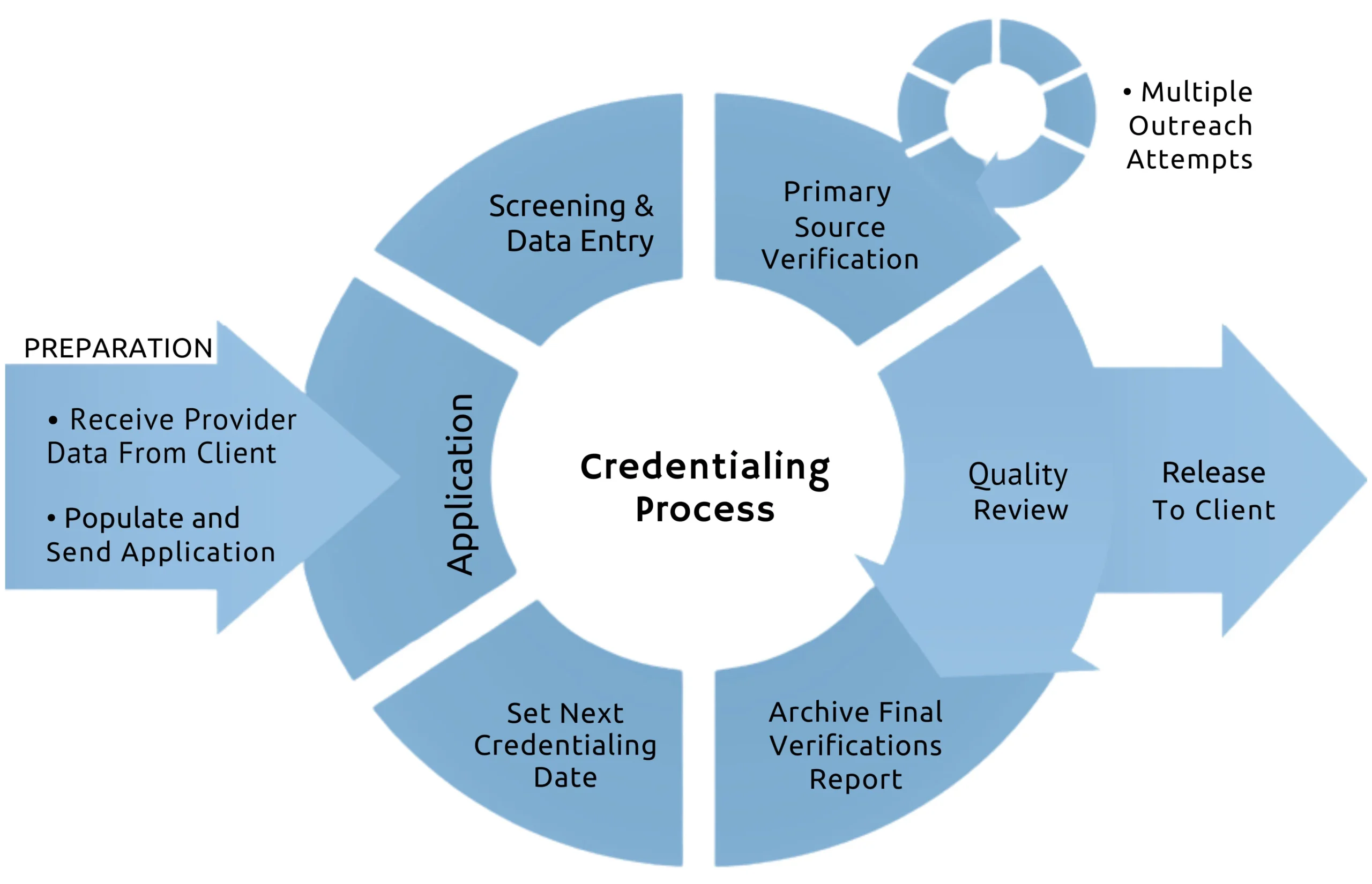
To guarantee that healthcare providers meet specific qualifications, our Credentialing Specialist will identify the necessary credentials. This step involves specifying the education, training, licensure, and other prerequisites essential for practicing within your healthcare organization.
We gather all the necessary an required documentation and verifying a professional’s work history, licensure, education, and board certifications. gathering complete and accurate information is essential for a successful credentialing application process.
A vital step in the credentialing process is to verify information directly from primary sources, including Licensing Boards, Medical Schools, and Previous Employers. This ensures the accuracy and reliability of the data provided by healthcare professionals.
Review and prepare all the required documents before sending the applications to each of the payers.
Regularly following up with healthcare professionals and all involved parties is essential to expediting the credentialing process. Communication is vital, and routine check-ins ensure instant resolution of any issues, keeping the process on schedule. Delays in the credentialing process often result from a lack of resources allocated and the lack of consistent, continuous follow-ups at every step of the process.
The completion of the process of reviewing a Provider’s credentials against national, standardized protocols and standards, such as those presented by NCQA and URAC.
Upon successfully completing credentialing, the provider is offered a standard network contract by the network payer.
The Benefits of Pro1RCM Professional Credentialing

Leveraging the Pro1RCM Credentialing Services allows healthcare organizations to focus on patient care and day-to-day operations, while Pro1RCM manages all aspects of the credentialing process in the background.
The Credentialing process is very complex and involves a tremendous amount of steps and actions that must be completed accurately and completely. The dedicated Pro1RCM Credentialing Specialists are dedicated to the credentialing, enrollment, and contracting processes for providers and healthcare groups, eliminating missed steps and delays in following up on every steps in the process. The pro1RCM Credentialing Specialists actively and diligently follow up on every step, every day which dramatically reduces the entire credentialing process timeframe and enables providers see patients much faster!
The average healthcare organization loses $9,000 every day a provider is unable to see patients. Leveraging an expert Credential Service Provider expedites the credentialing process enabling your providers to begin seeing patients much faster than trying to manage the rigorous credentialing process with inexperienced in-house employees that are also working on myriad of other tasks and responsibilities.
The Pro1RCM Credentialing Specialists have extensive training, certification, and experience in managing the complex tasks of credentialing clinical providers and healthcare organizations. Our credentialing specialists have proven processes that expedite each step and action in the credentialing process.


